Designing the Self-Report of Wellbeing in Pregnancy
Perinatal wellbeing is a public health priority with significant and long-lasting intergenerational effects. Every year, up to 15% of women are diagnosed with depression during pregnancy or within a year of giving birth. Perinatal depression affects women’s quality of life, birth outcomes, as well as children’s emotional, cognitive, behavioural and social development. Suicide is the leading cause of maternal mortality within the United Kingdom (UK).
Treatment and support, therefore, needs to be made available to those who require it, but in order to do so, effective programs of assessment and avenues of disclosure must be in place. In the context of the UK’s National Health Service (NHS), mental health screening during pregnancy is currently carried out verbally and using paper-based questionnaires completed in waiting rooms. However, it is estimated that at least 50% of perinatal depression cases go undiagnosed.
The work of Dr Kevin Doherty’s doctoral dissertation sought to support maternal mental health and wellbeing on a population scale, by establishing a case for the feasibility and design of mobile applications to support the self-report of psychological wellbeing and depression during pregnancy, facilitating access to care and support for those in distress.
Conducted under the supervision of Dr Gavin Doherty at Trinity College Dublin, this transdisciplinary project asked how technology shapes the self-report of wellbeing, how users engage and are engaged in the honest disclosure of mental health concerns, how health professionals might act upon reports of psychological wellbeing, and how technology might contribute to our evolving conception of wellbeing and its pursuit.
This was a highly complex context for research and design, combining the individual significance of wellbeing during pregnancy, the real-world and long-term use of technology by an at-risk user group, a public health system’s need to efficiently distribute resources, midwives’ diverse work practices, social expectations, societal stigma, as well as researchers’ motivations for data collection.
This work, therefore, entailed several years of close collaboration between HCI and public health researchers, pregnant women and a variety of health professionals including midwives, culminating in the first longitudinal clinical deployment of mobile technology for antenatal mental health screening.
Using BrightSelf, 355 pregnant women attending 14 NHS midwifery clinics across England provided 2,280 momentary and retrospective reports of their wellbeing in daily life over a period of 9 months. Women installed and engaged with this mobile application regardless of their age, education, number of children, marital status, employment status, past diagnosis of depression or level of wellbeing.
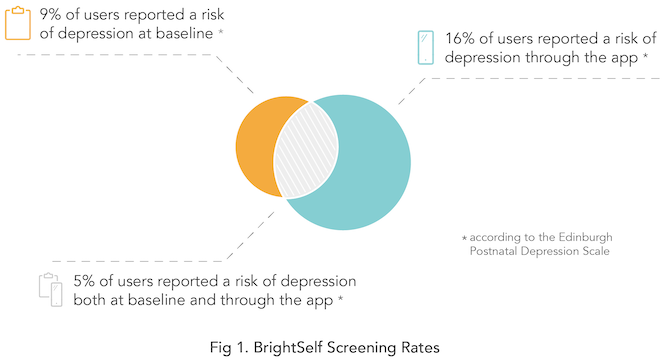
Thirty-nine women reported a risk of depression, self-harm or suicide using this technology and received immediate midwife support. Two-thirds of participants who received support in this way registered no risk of depression according to the standard screening methods employed in-clinic at baseline, and women spoke positively of the experience.
Visit Dr Kevin Doherty’s website to learn more about this project and its implications for antenatal public healthcare.
1 Comment on BrightSelf
Comments
Comments are closed.